By: Dr. Jerry Dreessen
 In a common case like a patient surviving a car accident, one of my first targets is to evaluate what's happened to the inside of their head. There's a difference between the effects of a slight rear end-- Was it a high or low speed impact? Was it a T-bone? Did they experience two car accident? Any kind of quick stop is going to cause everything to slide forward in the head and then come back-- what we call as "coup contrecoup". And it can disrupt the brain and may cause a mild hemorrhage. It can cause a little bit of bruising. Some people talk about feeling a little foggy after an accident- similar to walking into an attic with dust flying all around. That's what can happen to your brain when it starts to slap around inside the skull, just even from a mild car accident.
In a common case like a patient surviving a car accident, one of my first targets is to evaluate what's happened to the inside of their head. There's a difference between the effects of a slight rear end-- Was it a high or low speed impact? Was it a T-bone? Did they experience two car accident? Any kind of quick stop is going to cause everything to slide forward in the head and then come back-- what we call as "coup contrecoup". And it can disrupt the brain and may cause a mild hemorrhage. It can cause a little bit of bruising. Some people talk about feeling a little foggy after an accident- similar to walking into an attic with dust flying all around. That's what can happen to your brain when it starts to slap around inside the skull, just even from a mild car accident.
There are concussion protocols that we perform in the clinic. To process this type of patient starts with a questionnaire about:
* Cognitive abilities: What are the things that they can or can't do?
* Do they have a headache?
* Are they having a hard time focusing?
We also get into studying their emotional state as far as any feelings of SADNESS. Some people may have immediate reactions and seek help right away, while others come in for a consult weeks later.
THE 12 POINT CRANIAL NERVE CHECK
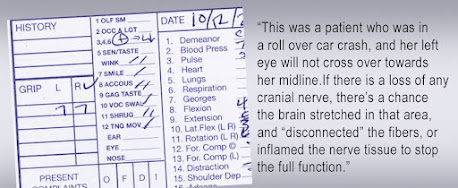
A standard exam is studying a CRANIAL NERVE CHECK. Not only do you have the brain sitting in the skull with a brain stem, which can be greatly affected with a whiplash scenario, but in the floor of the skull, there's 12 sets of nerves that come out and they perform different functions. This is often overlooked. There are many cases that do not show apparent concussion symptoms, but if they have one of the cranial nerves that doesn't work properly, this is a sure giveaway.We can start by helping that nerve system heal either through nutrition or through cognitive exercises but also eliminating the inflammation. Reading an MRI can be a challenge when looking for any mild type of inflammation in the brain- but with the proper diagnosis, we can reduce not only the concussion, but the possible post traumatic stress disorder and, and personality changes that can go along with it.
This standard process of reading the performance of the cranial nerve means studying 12 different nerves. This test helps determine if there's any kind of cranial nerve loss due to a car accident or sports injuries.
The first is the OLFACTORY nerve; this conveys the sense of smell. Some people can come in, barring the challenges of Covid symptoms and may already have loss of smell. Otherwise, if the accident may have affected their ability to smell, that's one signal that the olfactory nerve isn't functioning properly. (2) The next nerve that we check is the OPTIC nerve and that is what transmits information including blurry vision vs. the ability to focus on an object. Retinal reaction to light gets us the pupillary response.
The Double Impact of Post Concussion Disorder By: Ray Ciancaglini The first concussion was mild and it was a little bit of a headache and some fatigue. I got stunned but never been knocked out or knocked down, so that kind of fooled me here. Um, and then one week later in Syracuse, I got my bell rung again for the second time in one week. Only this time, it was a little bit more serious. And from being a well behaved high honor student, things changed. After that night, I started failing on all my courses, started sleeping excessively, and then I developed an attitude especially toward authority figures, and couldn't explain why. And, uh, this just lasted with me till I retired from boxing in 1974. From here, it got progressively worse. |
And then we have the cranial nerves three, four, and six, which are the OCULOMOTOR, TROCHLEAR and ABDUCENS (see chart). This is where the patient simply follows our finger with their eyes and we observe their field of gaze to find out if they're tracking properly. Depending on how the eyes perform during this test, we can determine which of those three cranial nerves and functioning properly. Next is the fifth cranial nerve called the TRIGEMINAL- that's the skin of the face. And as far as chewing (mastications). Oftentimes it's subjective information to ask if they have challenges chewing their food. Cranial nerve seven is the FACIAL nerve as far as what's involved in TASTE. Then, Cranial nerve eight is the VESTIBULAR COCHLEAR nerve- involving the hearing and balance. For this, we conduct the Trendelenburg test, where they stand on one foot and we just push them a little bit and see if they're able to balance.
 Then we employ the use of a tuning fork close to the ear and also touch the bone on the back of the head to see whether they can hear all of that. Any loss of hearing is indicative of an injured nerve. Cranial nerve #9 is checked by asking the patient if food tastes the same, or if it has changed in anyway, and if they have a developed a dry mouth. Cranial nerve #10 involves swallowing and also breathing. This is a significantly major nerve out of the whole system. We check the ability to swallow by by manually pressing the hand over the patient's throat and ask them to swallow.
Then we employ the use of a tuning fork close to the ear and also touch the bone on the back of the head to see whether they can hear all of that. Any loss of hearing is indicative of an injured nerve. Cranial nerve #9 is checked by asking the patient if food tastes the same, or if it has changed in anyway, and if they have a developed a dry mouth. Cranial nerve #10 involves swallowing and also breathing. This is a significantly major nerve out of the whole system. We check the ability to swallow by by manually pressing the hand over the patient's throat and ask them to swallow.
The ACCESSORY NERVE is #11 - where we instruct the patient to shrug their shoulders. We check for weakness or asymmetry. As the cranial nerve is split down the center, if the patient can only function on one side or another, this may indicate nerve paralysis, damage to the cranial nerve or the damage to the muscles of the neck.
The final (#12) cranial nerve is the HYPOGLOSSAL- tongue movement. By monitoring the patient's ability to push their tongue against their cheek.
CONCUSSION EXAMS (Part 2)- THE BENEFITS OF IMAGING: Concussion literature notes that in a Funduscopic exam, the retinal arterial-venous width will show as ASYMMETRIC (indicative of possible trauma). This is a potential response of the autonomic nervous system. Microcirculatory hemodynamics that are optically visible are useful in validating the treatment progress. (see complete review). Now that radiologists are using Doppler blood flow to examine eye disease, including systemic diseases (including Diabetes, Brain tumors, heart disease, sickle cell disease etc.) that affect the eye, we are hopeful that the ophthalmologic and neurological communities will start using this noninvasive technology as well to improve noninvasive and more rapid treatment of potential eye disorders, such as cancers of the eye, diabetes and glaucoma. Another future use will be to correlate the effect of decreased vascular pulsation in the production of cerebrospinal fluid that is removed by the cleansing glymphatic system is postulated as a contributing factor in degenerative neuromuscular disease. |
DR. JERRY DREESSEN is a chiropractor dedicated to the specialized work in Spinal Biomechanical Engineering Analytics and Case Management. He holds specialized credentials as a Trauma Team, Hospital care and Primary Spine Care in Mountlake Terrace, WA. He is the clinical director of an independent pain management practice called BACK TO ACTION CHIROPRACTIC the Executive Director for the Association of PEMF Professionals, a national organization for all PEMF users, and is a best selling author on Amazon with his book about Pain Management.
Ringside Review: Why the Boxing Commissioner Called to "STOP THE FIGHT" ? The photo was a stunning one-in-a-million shot of a moment in time (as captured by the sports photographer, Stephanie Trapp). Standing at the right place and at the right time, her lens managed to freeze multiple streams of explosive action that comprised Deontay Wilder completely obliterating Stiverne. The empty, worn out 'rag-doll' form of Stiverne's flacid body laid melted and dangling senselessly from the bottom rope. Center frame was the referee (Arthur Mercante Jr.) airborne on top of the highly charged and powerful Wilder, desperately grappling on the aggressive champ with his own unremarkable body. "Mercante responded vigorously to my raising the hand in the air at ringside-- that's the signal to 'STOP THE FIGHT!'... any more than this would be unconscionable". (See complete OP-ED feature)
The photo was a stunning one-in-a-million shot of a moment in time (as captured by the sports photographer, Stephanie Trapp). Standing at the right place and at the right time, her lens managed to freeze multiple streams of explosive action that comprised Deontay Wilder completely obliterating Stiverne. The empty, worn out 'rag-doll' form of Stiverne's flacid body laid melted and dangling senselessly from the bottom rope. Center frame was the referee (Arthur Mercante Jr.) airborne on top of the highly charged and powerful Wilder, desperately grappling on the aggressive champ with his own unremarkable body. "Mercante responded vigorously to my raising the hand in the air at ringside-- that's the signal to 'STOP THE FIGHT!'... any more than this would be unconscionable". (See complete OP-ED feature)
 2022 TRENDING INTEREST IN BRAIN HEALTH July 19, 2022- IPHA NEWS conducted a private interview with the co-developers of NEUROVINE - a portable headband using EEG (electroencephalogram) technology to measure brain waves. Meet CEO Ashleigh Kennedy, Ph.D., and CMO Matthew Kennedy, MD, MSc (co-founders of Neurovine) from Ottawa, Ontario, CA. who shares their objectives in support of concussion monitoring by measuring brain health as part of optimizing their recovery process. Neurovine offers this portable interactive monitoring program for athletes, students, professionals and anyone undergoing mentally strenuous work by “alerting them to take brain breaks before an activity becomes too strenuous”.
2022 TRENDING INTEREST IN BRAIN HEALTH July 19, 2022- IPHA NEWS conducted a private interview with the co-developers of NEUROVINE - a portable headband using EEG (electroencephalogram) technology to measure brain waves. Meet CEO Ashleigh Kennedy, Ph.D., and CMO Matthew Kennedy, MD, MSc (co-founders of Neurovine) from Ottawa, Ontario, CA. who shares their objectives in support of concussion monitoring by measuring brain health as part of optimizing their recovery process. Neurovine offers this portable interactive monitoring program for athletes, students, professionals and anyone undergoing mentally strenuous work by “alerting them to take brain breaks before an activity becomes too strenuous”.
 2022 STUDY OF INTRACRANIAL IMPACT DISORDERS - Concussions are viewed as a mild form of traumatic brain injuries and most frequently occur following an event that involves an acceleration–deceleration mechanism without actual injury to the head, such as whiplash, or the head striking an object. As we study these, researchers and clinicians are learning that these are fairly common, but often underdiagnosed. While the vast majority of people with concussions recover without obvious disability, people can end up with long-term cognitive, emotional and functional issues affecting quality of life – including memory issues and Alzheimer’s disease. Efforts to better predict outcome from head injuries by focusing on the age, sex, type of injury and acute assessments have led to some improvement, but still fail to predict or explain the variation in healing and outcomes. Studies in professional athletes have shown that about 80–90% are sufficiently recovered to return to playing within 7–10 days. But that means that 10-20% are not, and their recovery can take up to 3 times longer. Even taking into account variations in initial injury, this variation is difficult to explain or predict. (see complete feature by Dr. Roberta Kline)
2022 STUDY OF INTRACRANIAL IMPACT DISORDERS - Concussions are viewed as a mild form of traumatic brain injuries and most frequently occur following an event that involves an acceleration–deceleration mechanism without actual injury to the head, such as whiplash, or the head striking an object. As we study these, researchers and clinicians are learning that these are fairly common, but often underdiagnosed. While the vast majority of people with concussions recover without obvious disability, people can end up with long-term cognitive, emotional and functional issues affecting quality of life – including memory issues and Alzheimer’s disease. Efforts to better predict outcome from head injuries by focusing on the age, sex, type of injury and acute assessments have led to some improvement, but still fail to predict or explain the variation in healing and outcomes. Studies in professional athletes have shown that about 80–90% are sufficiently recovered to return to playing within 7–10 days. But that means that 10-20% are not, and their recovery can take up to 3 times longer. Even taking into account variations in initial injury, this variation is difficult to explain or predict. (see complete feature by Dr. Roberta Kline)
 CONCUSSION ON THE FIELD..."Miami, We Have a Problem!" OP-ED by: Dr. Michael Gruttadauria | 9/25/2022 - The Miami Dolphins prized quarterback Tua Tagovailoa sustained what was clearly a concussion. He was dazed and in trying to walk off the field, staggered and nearly collapsed. He was helped off the field and taken into the injury evaluation tent. You didn’t need to be a neurologist to see that he was shaken from hitting his head on the ground. Incredibly, the QB cleared the NFL Concussion Protocol and to everyone’s surprise, was allowed to play in the second half of the game. Many questions were raised about the injury following the game and everyone from the Dolphins coach, to their staff to Tua himself seemed to blame the entire incident on a back injury he said he sustained earlier in the game. (see complete issue)
CONCUSSION ON THE FIELD..."Miami, We Have a Problem!" OP-ED by: Dr. Michael Gruttadauria | 9/25/2022 - The Miami Dolphins prized quarterback Tua Tagovailoa sustained what was clearly a concussion. He was dazed and in trying to walk off the field, staggered and nearly collapsed. He was helped off the field and taken into the injury evaluation tent. You didn’t need to be a neurologist to see that he was shaken from hitting his head on the ground. Incredibly, the QB cleared the NFL Concussion Protocol and to everyone’s surprise, was allowed to play in the second half of the game. Many questions were raised about the injury following the game and everyone from the Dolphins coach, to their staff to Tua himself seemed to blame the entire incident on a back injury he said he sustained earlier in the game. (see complete issue)
 ON POST-CONCUSSION SYMPTOMS By: Dr. Robert L. Bard | The underreported cases of bowel permeability to toxins in concussion is likewise mostly anecdotal. The possibility of scanning the gut for increased blood flow following brain trauma may be easily performed as followed as a guideline for evaluation of concussion chronicity. As the bowel activity is regulated by the autonomic nervous system we may apply the same diagnostic endpoints as other physiologic norms. The response of the microvasculature in the retina provides a functional guideline as to the progression of brain trauma and concussion as measured by blood flow. The application of optical devices and sensors for physical (temperature, respiration, heart rate, blood pressure) chemical (pH, pO2, glucose, lipids, oximetry) and biological (antigens, antibodies, electrolytes, enzymes, inhibitors, metabolites, proteins) data with imaging (endoscopy, optical tomography, confocal microscopy) adds new classifications of metabolism in the altered state.
ON POST-CONCUSSION SYMPTOMS By: Dr. Robert L. Bard | The underreported cases of bowel permeability to toxins in concussion is likewise mostly anecdotal. The possibility of scanning the gut for increased blood flow following brain trauma may be easily performed as followed as a guideline for evaluation of concussion chronicity. As the bowel activity is regulated by the autonomic nervous system we may apply the same diagnostic endpoints as other physiologic norms. The response of the microvasculature in the retina provides a functional guideline as to the progression of brain trauma and concussion as measured by blood flow. The application of optical devices and sensors for physical (temperature, respiration, heart rate, blood pressure) chemical (pH, pO2, glucose, lipids, oximetry) and biological (antigens, antibodies, electrolytes, enzymes, inhibitors, metabolites, proteins) data with imaging (endoscopy, optical tomography, confocal microscopy) adds new classifications of metabolism in the altered state.
 A PARTNERSHIP WITH SPORTS MOMS Another key launch pad to this research program is his alliance with MOMS OF ATHLETES, co-architected by Dr. Roberta Kline (Women's Diagnostic Network) and Dr. Donna Febres. This educational advocacy group supports clinical care and preventive science to college level athletes. This unique alliance of professionals and moms are dedicated to finding the safest options in injury and pain care - with an emphasis on new solutions for concussion research and prevention. This includes the modern non-invasive (non-surgical) alternatives where possible. NCMOA also teams up with the professional pain and medical associations to collaborate on latest protocols and information on ground-breaking neurostimulation, electromagnetic, holistic/full-body solutions and wearable therapeutics plus the latest in non-radiation clinical imaging validation. (see complete details)
A PARTNERSHIP WITH SPORTS MOMS Another key launch pad to this research program is his alliance with MOMS OF ATHLETES, co-architected by Dr. Roberta Kline (Women's Diagnostic Network) and Dr. Donna Febres. This educational advocacy group supports clinical care and preventive science to college level athletes. This unique alliance of professionals and moms are dedicated to finding the safest options in injury and pain care - with an emphasis on new solutions for concussion research and prevention. This includes the modern non-invasive (non-surgical) alternatives where possible. NCMOA also teams up with the professional pain and medical associations to collaborate on latest protocols and information on ground-breaking neurostimulation, electromagnetic, holistic/full-body solutions and wearable therapeutics plus the latest in non-radiation clinical imaging validation. (see complete details)
Ringside Review: Why the Boxing Commissioner Called to "STOP THE FIGHT" ? The photo was a stunning one-in-a-million shot of a moment in time (as captured by the sports photographer, Stephanie Trapp). Standing at the right place and at the right time, her lens managed to freeze multiple streams of explosive action that comprised Deontay Wilder completely obliterating Stiverne. The empty, worn out 'rag-doll' form of Stiverne's flacid body laid melted and dangling senselessly from the bottom rope. Center frame was the referee (Arthur Mercante Jr.) airborne on top of the highly charged and powerful Wilder, desperately grappling on the aggressive champ with his own unremarkable body. "Mercante responded vigorously to my raising the hand in the air at ringside-- that's the signal to 'STOP THE FIGHT!'... any more than this would be unconscionable". (See complete OP-ED feature)
The photo was a stunning one-in-a-million shot of a moment in time (as captured by the sports photographer, Stephanie Trapp). Standing at the right place and at the right time, her lens managed to freeze multiple streams of explosive action that comprised Deontay Wilder completely obliterating Stiverne. The empty, worn out 'rag-doll' form of Stiverne's flacid body laid melted and dangling senselessly from the bottom rope. Center frame was the referee (Arthur Mercante Jr.) airborne on top of the highly charged and powerful Wilder, desperately grappling on the aggressive champ with his own unremarkable body. "Mercante responded vigorously to my raising the hand in the air at ringside-- that's the signal to 'STOP THE FIGHT!'... any more than this would be unconscionable". (See complete OP-ED feature)
 2022 TRENDING INTEREST IN BRAIN HEALTH July 19, 2022- IPHA NEWS conducted a private interview with the co-developers of NEUROVINE - a portable headband using EEG (electroencephalogram) technology to measure brain waves. Meet CEO Ashleigh Kennedy, Ph.D., and CMO Matthew Kennedy, MD, MSc (co-founders of Neurovine) from Ottawa, Ontario, CA. who shares their objectives in support of concussion monitoring by measuring brain health as part of optimizing their recovery process. Neurovine offers this portable interactive monitoring program for athletes, students, professionals and anyone undergoing mentally strenuous work by “alerting them to take brain breaks before an activity becomes too strenuous”.
2022 TRENDING INTEREST IN BRAIN HEALTH July 19, 2022- IPHA NEWS conducted a private interview with the co-developers of NEUROVINE - a portable headband using EEG (electroencephalogram) technology to measure brain waves. Meet CEO Ashleigh Kennedy, Ph.D., and CMO Matthew Kennedy, MD, MSc (co-founders of Neurovine) from Ottawa, Ontario, CA. who shares their objectives in support of concussion monitoring by measuring brain health as part of optimizing their recovery process. Neurovine offers this portable interactive monitoring program for athletes, students, professionals and anyone undergoing mentally strenuous work by “alerting them to take brain breaks before an activity becomes too strenuous”.
 2022 STUDY OF INTRACRANIAL IMPACT DISORDERS - Concussions are viewed as a mild form of traumatic brain injuries and most frequently occur following an event that involves an acceleration–deceleration mechanism without actual injury to the head, such as whiplash, or the head striking an object. As we study these, researchers and clinicians are learning that these are fairly common, but often underdiagnosed. While the vast majority of people with concussions recover without obvious disability, people can end up with long-term cognitive, emotional and functional issues affecting quality of life – including memory issues and Alzheimer’s disease. Efforts to better predict outcome from head injuries by focusing on the age, sex, type of injury and acute assessments have led to some improvement, but still fail to predict or explain the variation in healing and outcomes. Studies in professional athletes have shown that about 80–90% are sufficiently recovered to return to playing within 7–10 days. But that means that 10-20% are not, and their recovery can take up to 3 times longer. Even taking into account variations in initial injury, this variation is difficult to explain or predict. (see complete feature by Dr. Roberta Kline)
2022 STUDY OF INTRACRANIAL IMPACT DISORDERS - Concussions are viewed as a mild form of traumatic brain injuries and most frequently occur following an event that involves an acceleration–deceleration mechanism without actual injury to the head, such as whiplash, or the head striking an object. As we study these, researchers and clinicians are learning that these are fairly common, but often underdiagnosed. While the vast majority of people with concussions recover without obvious disability, people can end up with long-term cognitive, emotional and functional issues affecting quality of life – including memory issues and Alzheimer’s disease. Efforts to better predict outcome from head injuries by focusing on the age, sex, type of injury and acute assessments have led to some improvement, but still fail to predict or explain the variation in healing and outcomes. Studies in professional athletes have shown that about 80–90% are sufficiently recovered to return to playing within 7–10 days. But that means that 10-20% are not, and their recovery can take up to 3 times longer. Even taking into account variations in initial injury, this variation is difficult to explain or predict. (see complete feature by Dr. Roberta Kline)
 CONCUSSION ON THE FIELD..."Miami, We Have a Problem!" OP-ED by: Dr. Michael Gruttadauria | 9/25/2022 - The Miami Dolphins prized quarterback Tua Tagovailoa sustained what was clearly a concussion. He was dazed and in trying to walk off the field, staggered and nearly collapsed. He was helped off the field and taken into the injury evaluation tent. You didn’t need to be a neurologist to see that he was shaken from hitting his head on the ground. Incredibly, the QB cleared the NFL Concussion Protocol and to everyone’s surprise, was allowed to play in the second half of the game. Many questions were raised about the injury following the game and everyone from the Dolphins coach, to their staff to Tua himself seemed to blame the entire incident on a back injury he said he sustained earlier in the game. (see complete issue)
CONCUSSION ON THE FIELD..."Miami, We Have a Problem!" OP-ED by: Dr. Michael Gruttadauria | 9/25/2022 - The Miami Dolphins prized quarterback Tua Tagovailoa sustained what was clearly a concussion. He was dazed and in trying to walk off the field, staggered and nearly collapsed. He was helped off the field and taken into the injury evaluation tent. You didn’t need to be a neurologist to see that he was shaken from hitting his head on the ground. Incredibly, the QB cleared the NFL Concussion Protocol and to everyone’s surprise, was allowed to play in the second half of the game. Many questions were raised about the injury following the game and everyone from the Dolphins coach, to their staff to Tua himself seemed to blame the entire incident on a back injury he said he sustained earlier in the game. (see complete issue)
 ON POST-CONCUSSION SYMPTOMS By: Dr. Robert L. Bard | The underreported cases of bowel permeability to toxins in concussion is likewise mostly anecdotal. The possibility of scanning the gut for increased blood flow following brain trauma may be easily performed as followed as a guideline for evaluation of concussion chronicity. As the bowel activity is regulated by the autonomic nervous system we may apply the same diagnostic endpoints as other physiologic norms. The response of the microvasculature in the retina provides a functional guideline as to the progression of brain trauma and concussion as measured by blood flow. The application of optical devices and sensors for physical (temperature, respiration, heart rate, blood pressure) chemical (pH, pO2, glucose, lipids, oximetry) and biological (antigens, antibodies, electrolytes, enzymes, inhibitors, metabolites, proteins) data with imaging (endoscopy, optical tomography, confocal microscopy) adds new classifications of metabolism in the altered state.
ON POST-CONCUSSION SYMPTOMS By: Dr. Robert L. Bard | The underreported cases of bowel permeability to toxins in concussion is likewise mostly anecdotal. The possibility of scanning the gut for increased blood flow following brain trauma may be easily performed as followed as a guideline for evaluation of concussion chronicity. As the bowel activity is regulated by the autonomic nervous system we may apply the same diagnostic endpoints as other physiologic norms. The response of the microvasculature in the retina provides a functional guideline as to the progression of brain trauma and concussion as measured by blood flow. The application of optical devices and sensors for physical (temperature, respiration, heart rate, blood pressure) chemical (pH, pO2, glucose, lipids, oximetry) and biological (antigens, antibodies, electrolytes, enzymes, inhibitors, metabolites, proteins) data with imaging (endoscopy, optical tomography, confocal microscopy) adds new classifications of metabolism in the altered state.
 A PARTNERSHIP WITH SPORTS MOMS Another key launch pad to this research program is his alliance with MOMS OF ATHLETES, co-architected by Dr. Roberta Kline (Women's Diagnostic Network) and Dr. Donna Febres. This educational advocacy group supports clinical care and preventive science to college level athletes. This unique alliance of professionals and moms are dedicated to finding the safest options in injury and pain care - with an emphasis on new solutions for concussion research and prevention. This includes the modern non-invasive (non-surgical) alternatives where possible. NCMOA also teams up with the professional pain and medical associations to collaborate on latest protocols and information on ground-breaking neurostimulation, electromagnetic, holistic/full-body solutions and wearable therapeutics plus the latest in non-radiation clinical imaging validation. (see complete details)
A PARTNERSHIP WITH SPORTS MOMS Another key launch pad to this research program is his alliance with MOMS OF ATHLETES, co-architected by Dr. Roberta Kline (Women's Diagnostic Network) and Dr. Donna Febres. This educational advocacy group supports clinical care and preventive science to college level athletes. This unique alliance of professionals and moms are dedicated to finding the safest options in injury and pain care - with an emphasis on new solutions for concussion research and prevention. This includes the modern non-invasive (non-surgical) alternatives where possible. NCMOA also teams up with the professional pain and medical associations to collaborate on latest protocols and information on ground-breaking neurostimulation, electromagnetic, holistic/full-body solutions and wearable therapeutics plus the latest in non-radiation clinical imaging validation. (see complete details)
 |
| PSA from our Sponsor |
Disclaimer: MEDTECH REVIEWS* is a non-commercial user review of health-related technologies and is not intended as a marketing program for any device(s) featured in this video for evaluation. This presentation is for informational use only does not offer any direct medical claims whatsoever. Statements from all speakers herein are expressing their own unscripted views that do not reflect those of our producers. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment.