WOMEN'S DIAGNOSTIC NETWORK UPDATE
Mental Health 101: Treating Incontinence Starts With Overcoming The Stigma
By: Jessica Connell-Glynn, LCSW
Edited by: Roberta Kline, MD
Health issues are often linked to a range of emotional distress, but a major contributor to the progression of chronic issues such as urinary incontinence starts with the sufferer's instinct to conceal the problem. This reactive response from embarrassment and shame drives many women (both men and women) to hide their condition from their closest supporters as well as their physicians, making incontinence go unchecked and unaddressed. Over time, it is this level of clinical neglect that brings bladder health issues and urinary incontinence to grow into a more challenging health condition.[1]
Internalizing reactive shame plays a critical role in the effects of STIGMA and its self-propelling negative cycle, further driven by self-esteem issues, depression and hopelessness. From a 2002 World of Psychiatry report, both public and self-stigma may carry three components: stereotypes, prejudice, and discrimination. These elements are observed to be quite powerful in driving human activity and decision-making as they align with our sense of social acceptance, personal safety and survival.[2]
Treatment experts identify the critical progression of incontinence to start from the sufferer isolating themselves in secrecy. According to Daphna Ross, PT, owner of Women's Health and Healing Physical Therapy, Inc., "it is extremely embarrassing and uncomfortable for women to talk about this topic. They often hide it from friends or family but also from their doctors. This often contributes to worsening of their condition. At first it starts as a small leak and an annoyance but then it gets worse when left untreated; they require the use of pads, start limiting their social activities their exercise, or how long they're willing to be outside the home. The leakage will affect their quality of life. They often limit their fluid intake as well, which actually worsens their condition and causes other issues. It's really important to see the sufferers when it's just a small issue- women should know that there are tools to manage their condition and ensure that they don't go down this trajectory".
There have been many studies evaluating groups of sufferers of urinary incontinence directly reflecting emotional distress. Under varying conditions of functional loss, the investigative teams in these studies tend to conclude similar association between this physical impairment and levels of anguish and anxiety where the embarrassment of incontinence would often lead to self isolation- where seeking direct care or proper counsel is often compromised.[3]
References:
1) The impact of stigma on emotional distress and recovery from psychosis: The mediatory role of internalised shame and self-esteem https://pubmed.ncbi.nlm.nih.gov/28531822/
2) Understanding the impact of stigma on people with mental illness https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1489832/
3) Urinary Incontinence and Psychological Distress in Community-Dwelling Older Adults https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2827934/
MedReview: FEMALE INCONTINENCE EXPLAINED
Written by: Dr. Bobbi Kline
INTRODUCTION:
In my experience as an ObGyn, urinary incontinence is the unspoken secret among women. It affects up to 1 in 4 women, and this increases with age so that by age 65 up to 75% of women are affected [1]. And yet, most women never seek help. In a study published in 2013, 95% of women reported a negative impact on their quality of life, and yet 64% of the women had never received any medical help [2]. So often hidden out of shame, many women suffer in silence despite many efforts to raise awareness. Even those that are aware there is help may not seek it. What’s the point of speaking up when you fear it will only lead you down a path full of embarrassing conversations, invasive testing or procedures– and often does not produce effective or long-lasting results?
THE 'UNSPOKEN FEMALE DISORDER'
While urinary incontinence is most common in women over age 50, it can happen to women of all ages. More recent research is also showing that ethnicity plays a role. Sometimes the cause is temporary, as can happen with a urinary tract infection. Pressure on the bladder, as we see in pregnancy or from fibroids or other pelvic masses, can also lead to incontinence. Addressing the underlying issue typically leads to resolution of the urinary leakage.
But most commonly, the involuntary loss of urine is not so easily fixable. The causes of urinary incontinence are grouped into four different categories: urgency, stress, functional and overflow incontinence. Functional and overflow incontinence are typically due to non-bladder related causes, while urgency and stress incontinence are closely linked with dysfunction of the bladder or other structures in the pelvic floor.
The bladder is a sac made up of smooth muscle, and when it fills up with urine there is a reflex that results in release of that urine. Early in life we learn to control when those muscles contract, and thus control when we urinate.
URGENCY INCONTINENCE occurs when there is some loss of that control (3). This is often called “overactive bladder”, or OAB. Certain substances, such as caffeine or wine, or changes in hormones related to menopause, are known to aggravate this. But most often, we don’t know why this occurs. As a result, lifestyle or medication treatments are often less effective because we aren’t addressing the root cause.
STRESS URINARY INCONTINENCE is most often caused by trauma to the pelvic floor during childbirth, when the muscles that are designed to support the bladder are weakened (3). As a result, women leak urine when the bladder is put under pressure such as with coughing, sneezing, laughing or jumping. This is fairly common immediately after vaginal delivery, and many women will notice their symptoms improve with Kegel exercises designed to strengthen these pelvic floor muscles, along with the natural healing process. In my experience, many women are not sufficiently educated and supported in this. Or, as is especially the case with new moms, they are so busy taking care of everyone else that they neglect their own health needs.
Some women never fully recover, and even those that do often see the stress incontinence symptoms return later in life. And to make things even more challenging, often women have both urgency and stress incontinence. So women hide, often arranging their whole lives around avoiding leaking urine because they are ashamed to seek help. They change their exercise routine. They forego activities that bring them joy and pleasure, including sex. They buy pads and hope no one notices. They are always worried about a leak that reveals their shameful secret.
In my opinion, it’s part of a larger problem in how we view and treat women’s bodies. But fortunately, things are starting to shift thanks to technological advances in both our understanding and treatment. Even Personalized Medicine is yielding breakthrough insights into underlying causes. We are learning how each woman’s DNA related to pelvic floor muscles and collagen, and the DNA of her urinary microbiome, can impact her risk as well as the effectiveness of current treatments.
I am optimistic we may someday soon be able to truly tailor both prevention and treatment in a way that is much more accessible and effective in addressing urinary incontinence in women.
Why I wear Pull-Ups… By: Jesi Stracham When Depends became too baggy after my weight loss causing leaks and the pads would slide to the side, I switched to GoodNites brand children’s diapers. Immediately, my confidence was boosted with the cute designs and panty like fit. Even though I have my bladder well managed, I still wear them daily. With my active lifestyle I like the piece of mind that if I have an accident my wheelchair cushion and clothes will still be dry. I simply rip the diaper off, clean my downstairs “area” with a baby wipe, put a new diaper on and wheel on my way. Often times SCI survivors suggest Botox Injections and pharmaceuticals to help with my incontinence. I used both up until April 2017 when they quit working. I searched high and low for natural alternatives after realizing how well my body felt after getting off of the pharmaceuticals. The uncomfortable constipation and dry mouth ceased within days! Early summer 2018 I had a bladder study done. The nurse who perform the study shamed me for refusing to take the prescribed medicines. She put me in tears saying due to the amount of spasms my bladder has shrunk significantly. She continued on with a shame train because I refused pharmaceuticals after explaining they didn’t work and made me feel funny. She placed fear deep within my soul threatening that I would need a permanent catheter in my stomach with a bag or bladder augmentation (surgery where they take a piece of your bowel to make you bladder bigger) before I knew it. (see complete Blog entry) About the Author JESI STRACHAM is a trauma survivor on a mission to help individuals see the opportunity in their obstacles. She is the founder of Wheel With Me Foundation, the owner of Wheel With Me Consulting, and a fitness and growth coach. Through her struggles, she works for teaching individuals the power of our mindset. Jesi is an honest, authentic, America-loving athlete. Over the past several years, she has generated a significant following among both the spinal cord injury and able-bodied community. Her goal is simple: show the world there is an opportunity in their obstacles, restoring hope during life’s difficult moments. She helps people achieve their dreams through the importance of goal setting, taking control of what we have control over, and showing YOU what’s possible with consistent hard-work. |
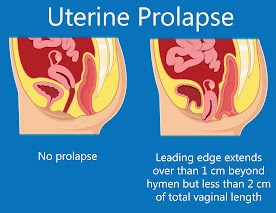
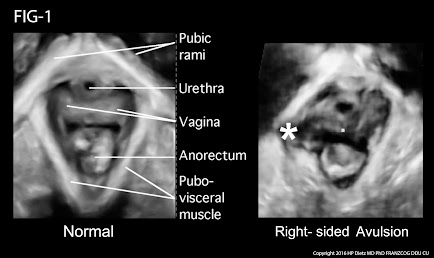
MRI has been used for years to image the prolapse of the pelvic organs but is being replaced by the 4D real time transperineal sonogram as it is quicker and instantaneously shows the tear in the muscular ring (levator sling) that is associated with the trauma of birth. This exam is done in the privacy of an office instead of an MRI center or hospital setting and may be completed in a few minutes by the physician or specially trained technician. The muscle bundle that supports the bladder is white on the sonogram while the tear is black and readily distinguished. During the examination the patient participates actively by bearing down or straining (Valsalva maneuver) to provide an exact measurement of the degree of the descent of the uterus, urethra, bladder or rectum.
Groundbreaking New Solution for Incontinence: Meet ELITONE
2/22/2022- Health and Healing 101 reviews the latest innovation in addressing female incontinence. A wearable medical device called ELITONE (by Elidah, inc.) hit the market in 2019, offering a non-intrusive incontinence treatment as an alternative to pads. Team Kolb shares their valuable insights on the creation of this remarkable device, while also discussing the road to achieving regulatory approval for product launch. (See complete article)
References
(2) Sensoy N, Dogan N, Ozek B, Karaaslan L. Urinary incontinence in women: prevalence rates, risk factors and impact on quality of life. Pak J Med Sci 2013;29(3):818-822
(3) Aoki, et al. Urinary Incontinence in Women. Nat Rev Dis Primers. ; 3: 17042
CONTRIBUTORS

JESSICA CONNELL-GLYNN, LCSW, CPC, CEC - (Mental Health Dir.)
 DAPHNA ROSS, PT, PRPC, WCS (Guest contributor / technical advisor)
DAPHNA ROSS, PT, PRPC, WCS (Guest contributor / technical advisor)Disclaimer: The information (including, but not limited to text, graphics, images and other material) contained in this article is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice or scientific claims. Furthermore, any/all contributors (both medical and non-medical) featured in this article are presenting only ANECDOTAL findings pertaining to the effects and performance of the products/technologies being reviewed - and are not offering clinical data or medical recommendations in any way. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, never disregard professional medical advice or delay in seeking it because of something you read on this page, article, blog or website.