DIABETIC NEUROPATHY AND THE GLOBAL PANDEMIC

DIABETIC NEUROPATHY
Diabetic neuropathy is comprised of various types of nerve damage associated with diabetes mellitus. Symptoms can include weakness, sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. [2] The different types of diabetic neuropathy include Peripheral neuropathy --nerve damage that typically affects the extremities-feet, legs or hands). Another type is Autonomic neuropathy which is comprised of damage to nerves that control your internal organs. Focal (damage to single nerves) and Proximal neuropathy- a rare and disabling type of nerve damage in your hip, buttock, or thigh. [3]
1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7096070/
2) https://en.wikipedia.org/wiki/Diabetic_neuropathy
3) https://en.wikipedia.org/wiki/Diabetic_neuropathy
 |
| Sponsored AD |
Meet our newest Functional and Holistic Health Expert- Dr. Robert Kornfeld. In this issue, IPHA NEWS features Dr. Kornfeld's advanced knowledge in the topic of Type-2 diabetes. He is a seasoned researcher and therapist in functional medicine and is well-published and broadcast for his expanded insight on chronic disorders. Originally promoted as a certified Podiatrist, he employs this specialized study to add to his diagnostic insight to support the management of chronic disorders while building prevention and wellness care for his many patients.
BATTLING DIABETES WITH FUNCTIONAL MEDICINE
From an interview with Dr. Robert Kornfeld
STRATEGIC INTERVENTION OF THE DIABETIC PATIENT
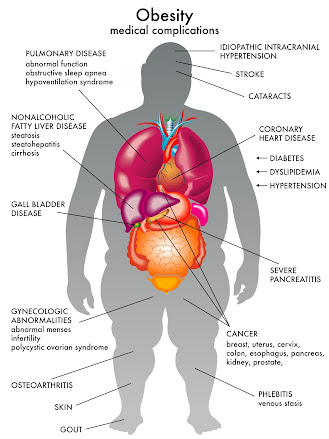
Too many walk into doctor's offices in this day and age with open wounds that don't heal. And now, we have a whole new subspecialty in podiatry called wound care and it exists because it's really necessary. How many antibiotics can you give them before it starts to wreak havoc on their kidneys, on their microbiome and essentially, on their immune system? In addition, there are larger problems with bone infection and eventual amputation. We have a fine line that we must walk with these patients because unfortunately diabetes also damages kidneys, it can damage the retinas. There is a lot of secondary pathology that we can avoid with proper understanding of what's going on in this patient’s epigenetics. I’ll also look into possible DNA mutations that interfere with normal healthy immune function and if we find them, we can intervene on behalf of those mutations and change the dynamics of that patient's physiology.
The very first thing I do as a functional medicine specialist is to have the patient JOURNAL their diet. Even though they're supposedly well controlled (medically), I get back diet journals that are 60, 70, sometimes 80% carbohydrate. Now we know why the patient is a diabetic. So I explain to them your A1C reading is an average. If you spike up and then fall below and spike up and fall below, it may come out a decent average over time, but every time your blood sugar spikes, there are certain things that happen.
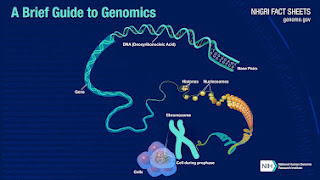
ESSENTIALS OF GENOMIC TESTING By: Dr. Roberta Kline DNA (deoxyribonucleic acid) makes up the genes that contain the blueprint for how our bodies operate ‐ from energy production in mitochondria to walking and breathing, from cellular health to digesting food, from thinking and running to protection from viruses, how we age and more. While humans are 99.9% alike in our DNA, it's the difference in that 0.1% that makes us each unique. Much of that difference comes from millions of small changes in our DNA. Genomic testing focuses on these small changes in DNA called single nucleotide polymorphisms (SNPs) that potentially predispose to disease or problems with medications by altering the body's biochemistry. But knowing about these potential areas of weakness is just the first step. The powerful part is that we know how to modulate their impact, thus potentially changing the outcome by reversing course, delaying onset or even preventing a disease process altogether. By decoding the instructions contained in DNA, each person becomes empowered with their own operating manual as to what they need for health. They can let go of the struggle as their blueprint guides them to the diet, lifestyle, exercise, supplements and medications that are best suited to their genes. And because we are only human, when life throws a curveball, having this personalized roadmap helps to get back on track much faster and with more precision. ▪NUTRIGENOMICS evaluates DNA to provide personalized diet, lifestyle, supplement and exercise recommendations for prevention and disease management strategies. ▪ONCOGENOMICS is a sub-field of genomics that characterizes cancer-associated genes. It focuses on genomic, epigenomic and transcript alterations in cancer. ▪PHARMACOGENOMICS evaluates DNA to provide personalized medication guidance for current and/or future medications. |
IMPACT OF DIABETES ON THE BRAIN
By Marilyn Abrahamson, MA,CCC-SLP - CBHC
HOW DIABETES AFFECTS COGNITIVE FUNCTION
Research has shown that people with diabetes are more likely to experience cognitive decline with an increased risk for Alzheimer's disease and other types of dementia. Diabetes mainly affects four cognitive domains; attention, processing speed, executive function, and memory. Both type 1 and type 2 diabetes can cause these cognitive problems, which suggests that high blood sugar, wide glucose excursions, and insulin resistance all play important roles.
HOW DIABETES AFFECTS THE BRAIN
There are several ways in which diabetes can harm the brain. High blood glucose, or wide glucose excursions cause:
● Oxidative stress: causing certain types of toxins called free radicals to build up in the blood.
● Inflammation: can damage blood vessels, and impair brain function.
● Insulin resistance: a common feature of type 2 diabetes, which can disrupt and damage important neural pathways in the brain needed to function normally.
BRAIN IMAGING RESEARCH has shown that diabetes can also cause changes in the brain’s structure. Certain areas, like the hippocampus, frontal lobes, and basal ganglia, are particularly vulnerable to damage, which can result in reduced brain volume (size) as a result of the reduction of gray matter. These changes may also explain why people with diabetes often experience cognitive problems and have a higher risk of developing Alzheimer’s disease and other types of dementia.
PROTECTING THE BRAIN & MANAGING DIABETES
Detecting and managing diabetes early is crucial for minimizing its impact on the brain and how it functions. Lifestyle choices that support and healthy body and brain, such as regular exercise, a healthy diet, and maintaining a healthy weight, are important for controlling glucose and for managing diabetes. Medications, like insulin and other drugs, can also help regulate glucose levels. Taking care of cardiovascular health by controlling blood pressure and cholesterol is essential because these factors contribute to both diabetes and cognitive decline.
*See other BRAIN HEALTH ARTICLES by Marilyn Abrahamson
● What is Brain Training? [article & video]
● The Doorway Effect – Why We Forget Why We’ve Walked Into a Room [article & video]
● Post-Covid Brain Fog vs. Work Performance
MARILYN ABRAHAMSON, MA, CCC-SLP : As a Brain Health Education Specialist at Ceresti Health, Marilyn offers initiatives that supports education and empowerment of family caregivers and she is part of the editorial team at the Ceresti monthly newsletter- producing all brain health education & coaching programs for caregivers. Marilyn's prior work is as a NJ Licensed Speech-Language Pathologist since 1987 and is an Amen Clinics Certified Brain Health Coach.
 |
Insulin-Dependent & Non Insulin-Dependent Diabetes Mellitus. |
Included in the many health areas to consider with diabetes, there's also an issue with immune function. We find with many diabetics, a problem in the ratio of copper and zinc. In the standard American diet, copper levels go way up and zinc levels begin to drop and the immune system goes to sleep. To reawaken it, we need to find out what's going on in that ratio- and in many cases, we can (carefully) supplement with an appropriate level of zinc. On the other hand, when you give a patient too much zinc, this can elevate some of the B vitamins to the point where they can cause neuropathy. So everything has to be managed.