VIDEO SPOTLIGHT: PEMF 101
Dr. Robert Bard, producer of IPHA's MedTech Reviews asks a frequently asked concern about "How safe is PEMF therapy?" See his interview with Dr. Jerry Dreessen who educates on its history (seed germination, treating injuries in animals) and its transition to working on human disorders.
ELECTROMAGNETICS VS. SOFT TISSUE INJURY
Written by: Josh Schueller, PT / Edited by: Dr. Robert L. Bard
Sprains, strains, and muscle soreness can cause many to be limited or bed ridden for weeks into months. This physical and emotional strain can be detrimental for a person. Even though there may be no fractures or major injury the time off from work and life can a major roadblock. Common treatments prescribed by health care professionals is rest, ice, medications and time. These treatments may take weeks to months for full recovery. Many people will try and rush their recovery and come back too soon or not when fully recovered and could lead to more injuries.
THE HEALING OPTIMIZER OF ELECTROMAGNETICS
One such slip-n-fall injury occurred in my immediate area: a 47 year old male who fell on the ice while walking his dog. He immediately had pain and swelling with moderate bleeding in his left elbow. He went to the emergency department for X-Ray which came back negative. The mechanism of injury was his elbow smashing into the icy driveway. He had significant pain 8/10, swelling over the olecranon process, and significant decrease in range of motion of elbow flexion and extension and was told that due to the musculoskeletal injury recovery could take weeks.
(Click to continue in section B)
EXTRA: Ultrasound Tracking of Hair Regen Progress from PEMF by: Dr. Robert L. Bard When a patient comes in for hair loss treatment, the clinician will assess the scalp for the specific types of hair loss, the most common being Androgenetic Alopecia. This is also known as male or female pattern baldness that occurs gradually from either a thinning from the crown, receding hairline or thinning from the part. There are also other types of hair less including Sudden Hair Loss (Alopecia areata) which occurs when the body’s immune system attacks hair follicles or can have sudden fallout due to systemic shock or stress. Recently, temporary hair loss has been linked to Covid-19 infection where those recovering may find that their hair is falling out in large clumps. According to the American Academy of Dermatology Assoc, fever is a common symptom of COVID-19 and temporary hair loss is normal after a fever. While many people think of this as hair loss, it’s actually hair shedding. The medical name for this type of hair shedding is Telogen Effluvium. It happens when more hairs than normal enter the shedding (telogen) phase of the hair growth lifecycle at the same time. A fever or illness can force more hairs into the shedding phase. It is observed that Treatment may address any underlying conditions and includes topical scalp medications. This form of hair loss from COVID 19 is extremely common. It is reversible by using the ultrasound in the skin. You can see that the hair follicles are in the formative stage, which means the follicles are not dead or dying, but they're available for regrowth. So the Massive hair loss condition will not be permanent. When we look at the skin under a trichoscope, we can obtain a quantifiable image before and after treatment in the scalp. The trichoscope is a way to visualize the quality of the hair shaft as to see if they're dying, If they're thick or thin or growing and perhaps more importantly, it measures the number of hair shafts per square centimeter. This number will be used to evaluate treatment at a four to six month interval for effectiveness. While a dermatologist can usually see just the top of the skin, the high resolution ultrasound technology sees the surface of the skin, the hair shaft and hair follicles as well as the blood vessels in the subdermal region that are necessary to nourish the hair follicles. The image insert showing the three white arrows against the diagonal black cavities. is a demonstration of hair follicles at the base with the small white arrows and the hair shafts with the larger white arrows extending from the subdural tissue into the outer skin. The white line is the gel on the scalp and the very tiny black line beneath it, which is 1/10 millimeter thick is the epidermis. The gray area on top is the top layer of the dermis whereas the wider area below is the deep layer of the dermis. The white arrows refer to the hair shaft, which in the center hair shaft extend down to the base of the hair shaft in the hair follicle from which the hair is reborn. PEMF treatment increases blood circulation in many disorders, especially diabetes and other diseases such as scar formation and assists in healing wound sites. Since PEMF is approved for treating major depressive disorders, and the ultrasound probe is placed on the scalp, we noticed that people who are using the treatment for depression were noticing that the lost hair or the thinning area on this scalp we're re-growing. This led us to researching for PEMF response and there are articles showing its success on a global scale. Since this is a non-contact and safe technology, we are able to visually look at the scalp and hair shaft (as in the left slide) we can look underneath the skin with high resolution ultrasound to make sure that the follicles are viable before going on a course of perhaps prolonged treatment. And then seeing if the Doppler blood flow technology reveals an increase In the circulation needed for hair growth in the deeper portion of the dermis and subdermal tissue compartment. The demonstration of increased or new blood flow ensures that the treatment will be successful at a later date when it can be seen visually on the surface of the skin. Additionally, Inflammation of the hair follicle, which is below the surface of the skin is quickly diagnosed with ultrasound. So a course of antibiotic treatment may be instituted immediately to correct the abnormality before other treatments are instituted. * Check out additional stories like this from AXIOBIONICS.com |
ELECTROMAGNETICS VS. SOFT TISSUE INJURY CONTINUED
Instead of the traditional treatment model that the emergency department prescribed, he chose to receive PEMF treatments instead. (see PEMF (Pulsed Electromagnetic Field Therapy) info). Theoretically, PEMF devices have been marketed to use the body’s own magnetic field to improve healing from a cellular level and has been reported to decrease recovery time and improve the healing process.
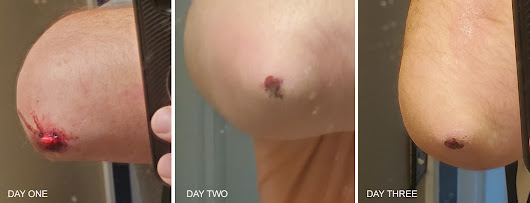
Here are the documented results from 3 days of healing from the use of PEMF therapy:
Day 1- pain levels 8/10. Moderate swelling and decrease left elbow ROM. Unable to lift or use left upper extremity with ADLS. PEMF treatment consisted of an undisclosed brand for 15 min at an intensity of 8.5 twice a day (one in morning one at night)
Day 2- Pain levels 3/10, with no swelling and full ROM in the left elbow. Able to use left upper extremity with most activities with mild pain (3/10). Day 2 treatments same as day 1.
Day 3- pain levels 0/10 significant healing in skin injury. Able to achieve full ROM in left elbow without pain or restrictions. Full strength returned. Same treatment as previous days.
Day 4 - fully recovered to full activates without restrictions. Mild scabbing over left elbow
EPILOGUE
During this treatment period the subject did not take any medications-prescribed or over the counter for pain. He did not use ice or compression to the injured area. In order to obtain clearer results his only treatment was PEMF for 4 days. A normal recovery time of weeks was decreased to days. The cost is minimal and full recovery was achieved. While traditional treatment contain value, the increasing use of alterative options is gaining in popularity because of its effectiveness and safety. Maximizing your body’s own recovery capabilities instead of medications (with possible side effects) is a far more efficient way to recovery from injuries.
**Always consult with a trained medical professional before using any treatment. Results may vary***
DISCLAIMER: In pursuit of journalistic integrity and scientific reporting, all reports, clinical findings and testimonials listed reflect our policy of complete IMPARTIALITY, whereby performance reviews of any product/technology - and are managed to be free from any commercial claims. Any/all sourced materials referring to brands are citing credit of source and is not to be misconstrued as branding and marketing.
 ROBERT L. BARD, MD, PC, DABR, FASLMS - Dr. Bard is recognized for his specialized work in advanced cancer diagnostic imaging. He co-founded the 9/11 CancerScan program to bring additional diagnostic support to all first responders from Ground Zero. His main practice in midtown, NYC (Bard Diagnostic Imaging- www.CancerScan.com) uses the latest in digital imaging technology and has been also used to help guide biopsies and in many cases, even replicate much of the same reports of a clinical invasive biopsy. Imaging solutions such as high-powered sonograms, Power Doppler Histogram, sonofluoroscopy, 3D/4D image reconstruction and the Power Doppler Histogram are safe, noninvasive, and do not use ionizing radiation. It is used as a complement to find anomalies and help diagnose the causes of pain, swelling and infection in the body’s internal organs while allowing the diagnostician the ability to zoom and ‘travel’ deep into the body for maximum exploration. (DrRobertBard.com)
ROBERT L. BARD, MD, PC, DABR, FASLMS - Dr. Bard is recognized for his specialized work in advanced cancer diagnostic imaging. He co-founded the 9/11 CancerScan program to bring additional diagnostic support to all first responders from Ground Zero. His main practice in midtown, NYC (Bard Diagnostic Imaging- www.CancerScan.com) uses the latest in digital imaging technology and has been also used to help guide biopsies and in many cases, even replicate much of the same reports of a clinical invasive biopsy. Imaging solutions such as high-powered sonograms, Power Doppler Histogram, sonofluoroscopy, 3D/4D image reconstruction and the Power Doppler Histogram are safe, noninvasive, and do not use ionizing radiation. It is used as a complement to find anomalies and help diagnose the causes of pain, swelling and infection in the body’s internal organs while allowing the diagnostician the ability to zoom and ‘travel’ deep into the body for maximum exploration. (DrRobertBard.com) JOSH SCHUELLER, PT has dedicated his life's work to the support and treatment chronic pain and disorders with non-invasive, safe, effective treatment solutions. He is the current VP of Clinical Operations and Business Development at AxioBionics LLC. and the Clinical Director for Orthopedic Physical Therapy Clinics (Rockford, MI). As an active member of APTA, he holds advanced certification in Physical Therapy treatment techniques including the McKenzie method of patient empowerment. He has over 20+ years experience in the treatment of neurological conditions such as Spinal Cord Injury, Traumatic Brain Injury, CVA, Cerebral Palsy etc. In 2021, Josh is elected a clinical advisory role and educational advocacy for IPHA (Integrated Pain Healers Alliance) and has published research articles in pain management.
JOSH SCHUELLER, PT has dedicated his life's work to the support and treatment chronic pain and disorders with non-invasive, safe, effective treatment solutions. He is the current VP of Clinical Operations and Business Development at AxioBionics LLC. and the Clinical Director for Orthopedic Physical Therapy Clinics (Rockford, MI). As an active member of APTA, he holds advanced certification in Physical Therapy treatment techniques including the McKenzie method of patient empowerment. He has over 20+ years experience in the treatment of neurological conditions such as Spinal Cord Injury, Traumatic Brain Injury, CVA, Cerebral Palsy etc. In 2021, Josh is elected a clinical advisory role and educational advocacy for IPHA (Integrated Pain Healers Alliance) and has published research articles in pain management.  Dr. JERRY DREESSEN is both Trauma Team Qualified and Hospital Qualified treating chiropractor in Mountlake Terrace, WA. He is the Executive Director for the Association of PEMF Professionals- the largest professional PEMF organization in the United States. AOPP attracts the most principled and accomplished PEMF user- setting standards by providing certification for all PEMF users, as well as Continuing Education (CEU's) for all members to maintain best practices and techniques. (www.backtoaction.com)
Dr. JERRY DREESSEN is both Trauma Team Qualified and Hospital Qualified treating chiropractor in Mountlake Terrace, WA. He is the Executive Director for the Association of PEMF Professionals- the largest professional PEMF organization in the United States. AOPP attracts the most principled and accomplished PEMF user- setting standards by providing certification for all PEMF users, as well as Continuing Education (CEU's) for all members to maintain best practices and techniques. (www.backtoaction.com)Disclaimer: The information (including, but not limited to text, graphics, images and other material) contained in this article is for informational purposes only. No material on this site is intended to be a substitute for professional medical advice or scientific claims. Furthermore, any/all contributors (both medical and non-medical) featured in this article are presenting only ANECDOTAL findings pertaining to the effects and performance of the products/technologies being reviewed - and are not offering clinical data or medical recommendations in any way. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen, never disregard professional medical advice or delay in seeking it because of something you read on this page, article, blog or website.